From Today Online:
Singapore — He was diagnosed with glaucoma in 2014, but 61-year-old Mr Ismail Busri does not know when the insidious eye disease first crept up on his left eye. Characterised by progressive damage to the optic nerve and loss of vision, glaucoma is one of the leading causes of blindness worldwide.
“I was very surprised when the doctor told me I had glaucoma as no one else in my family has it. By then, about half of the vision in my left eye was already damaged. Luckily, I did not wait too long to see a doctor or my vision loss would be worse,” said Mr Ismail, who also has myopia.
Mr Ismail suffers from primary open angle glaucoma (POAG), the most common type of glaucoma affecting three in 200 adults here and two-thirds of all glaucoma patients in Asia, said Associate Professor Cheng Ching Yu, clinician scientist at the Singapore Eye Research Institute (SERI) and Singapore National Eye Centre (SNEC).
Due to its lack of obvious symptoms in the early stages, this type of glaucoma has a four-fold likelihood of going undiagnosed compared with another form, primary angle closure glaucoma (PACG), until it hits the moderate to late stages, said Assoc Prof Cheng.
In the acute form of PACG, symptoms such as eye pain, headaches, nausea and blurred vision tend to occur suddenly.
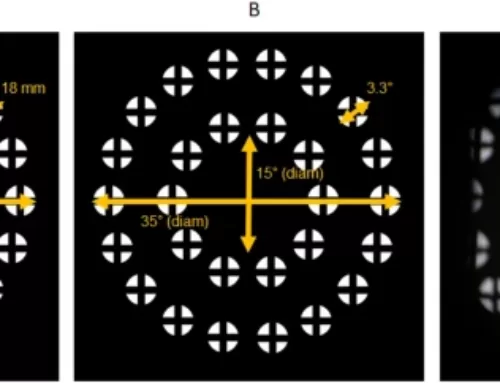
“In POAG, the patient loses vision silently and insidiously at first, leading to a decreased field of view and irrecoverable vision loss. One only notices it when a significant amount of damage has already occurred,” added Adjunct Associate Professor Shamira Perera, senior consultant ophthalmologist at SNEC’s Glaucoma Department.
Field of view is one’s entire scope of vision, which includes the central and side vision. But a new local study by researchers from SNEC and SERI may potentially help doctors detect the eye disease at an earlier stage.
Published last month in Scientific Reports, it is the first study demonstrating higher odds of POAG among people who have both high eye pressure and myopia. Previous studies looked at each factor separately as risk factors for the eye disease.
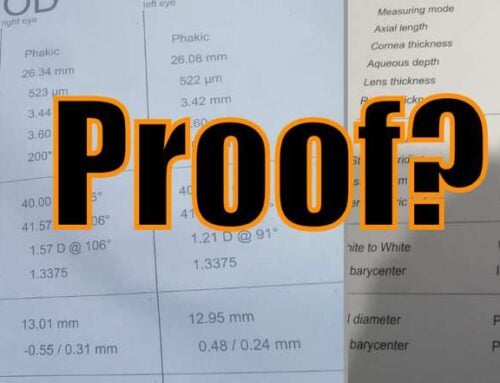
The researchers looked at 9,422 participants, of which 213 had POAG. Those with moderate to high myopia (above 300 degrees) and high eye pressure were more than four times more likely to develop POAG, compared with those without myopia and high eye pressure.
Patients with longer axial length and high eye pressure were 16 times more likely to have POAG, compared with those with shorter axial length and lower eye pressure.
Eyes with myopia tend to have longer axial length, which refers to a specific measurement from the front to the back of the eye.
Assoc Prof Cheng, the principal investigator for the study, said the findings are particularly relevant for the Asian population and in Singapore, considering the prevalence of myopia here. Myopia has been on an uptrend across all ethnic groups here in the last two decades. At present, about 80 per cent of 18-year-olds are short-sighted.
“These findings suggest that more regular screenings may be targeted at individuals who present with high eye pressure and myopia. Should the disease occur, this approach may potentially help to detect POAG at an even earlier stage,” said Assoc Prof Cheng.
There is currently no cure for glaucoma, but detecting and treating the disease early can stave off blindness, added Adjunct Assoc Prof Perera. Treatments ranging from medications and laser therapy to surgery work by reducing eye pressure to control the disease’s progression.
Assoc Prof Cheng suggested regular eye examinations for people with high myopia of over 600 degrees and a family history of glaucoma, upon reaching the age of 40.
For adults with myopia, and who are found to have increased eye pressure, it may be advisable to undergo yearly comprehensive eye screenings by an ophthalmologist, said Professor Saw Seang Mei, head of the Myopia Unit at SERI and the study’s co-investigator.
Fortunately for Mr Ismail, prompt treatment has saved his remaining sight for the time being, allowing him to continue with his 12-hour shift work in the petroleum industry. He underwent laser treatment and surgery last year to control the high eye pressure in his left eye. “I know that glaucoma is incurable. Thankfully it has not affected my life so drastically as my condition is under control. At the moment, I’m praying hard that it won’t affect my other eye,” he said.
Advances in modern medicine to deal with acute symptoms is often impressive.
It also may be worth bearing in mind that you can reduce your risk of the most common forms of glaucoma by as much as 300%, by reducing your high myopia. Individuals who are not myopic have been found to have three times lower risk of developing glaucoma (see the studies on the subject).
How does the saying go? An ounce of prevention, something something …
Cheers,
-Jake